
Affordable Care Act navigator Nini Hadwen helps Floridians shop for health insurance in October.
Joe Raedle/Getty Images
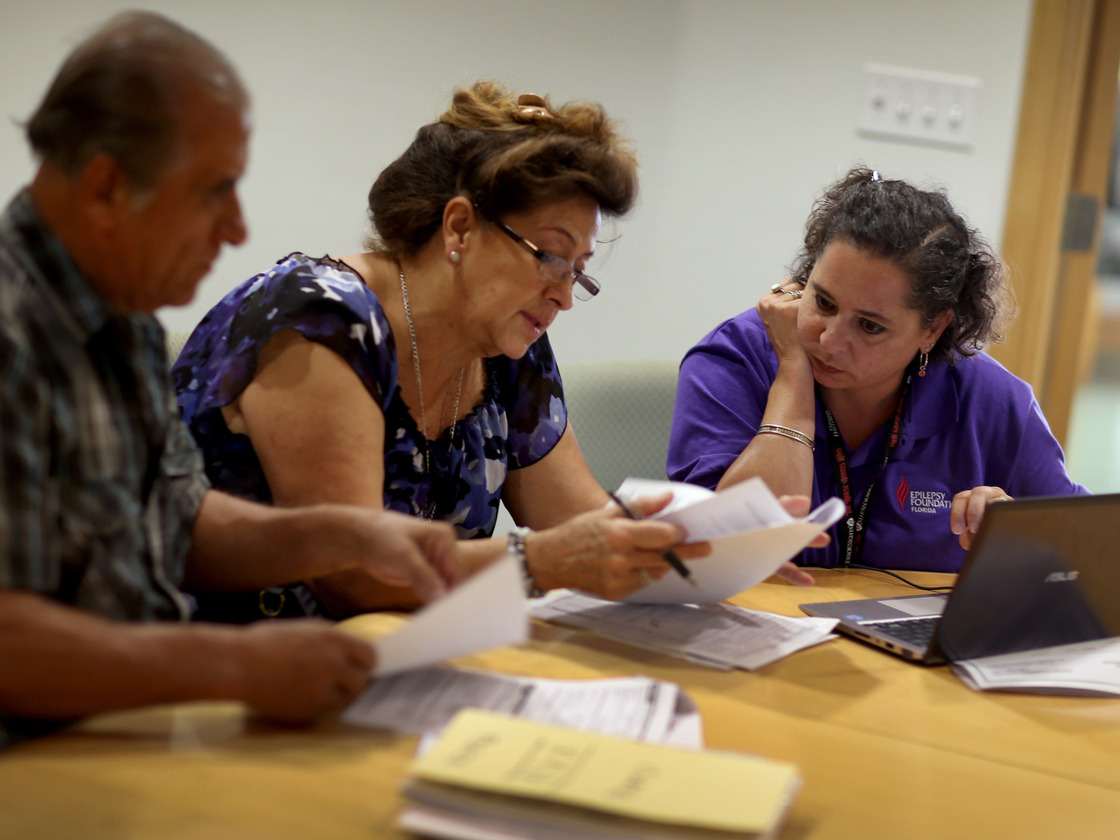
Affordable Care Act navigator Nini Hadwen helps Floridians shop for health insurance in October.
Joe Raedle/Getty Images
With just a few weeks left before a deadline to get health coverage, lingering bugs lurk in the part of HealthCare.gov that you can't see. And time is running out to get things right.
Consumers have to sign up for a health insurance exchange — and pay their first month's premium — by the end of December if they want coverage in January.
"The short time period presents a number of challenges," says Robert Zirkelbach, a spokesman for America's Health Plans, an insurance industry trade group.
The 834 forms — electronic files sent from HealthCare.gov's back end to insurance companies — must have accurate and complete data in order for a consumer to be considered fully enrolled.
The White House is projecting confidence: "We have a team of experts working both through technological fixes but also through some elbow grease going through and confirming that that information is conveyed accurately and completely, to confirm that they'll be signed up for health care and eligible to get covered on January 1st," White House Deputy Press Secretary Josh Earnest said Wednesday.
But the Obama administration estimates one in 10 forms are still problematic, an improvement from one in four bad forms in October and November.
And challenges go beyond processing. Since health plans won't start coverage until they're paid, anyone mailing in a check will have to get it in quickly.
"If an enrollee does not pay their first month's premium by December 31, their enrollment will be void. So far, the health plans I have spoken to have seen only about 20% percent of their enrollees pay their premium," health industry consultant Bob Laszewski wrote in his blog Thursday.
"The situation everyone wants to avoid is a situation in which consumers think they're enrolled when they're not. Or the situation where they find out that they're not enrolled when they try to schedule an appointment to see a doctor," Zirkelbach says.
Then, there's the work of reconciling the government enrollment records with the data received by insurance companies.
"I don't think you can be confident that everyone who is enrolled will have a plan until we can do a reconciliation between the government records and the insurance company records," Laszewski told NPR.
The work of reconciling files just got started Wednesday, when health officials sent spreadsheets of their latest enrollment data to insurers to cross-check records. Zirkelbach says it's a significant step.
"It will for the first time give us the size and scope of the technical challenges that exist," he says. For all the focus on technology in recent weeks, Health and Human Services Secretary Kathleen Sebelius says that reconciliation work is getting done manually.
"We are in the process of actually hand-matching individuals with insurance companies," she told lawmakers in a Wednesday hearing.
With the deadlines getting closer and December enrollments surging ahead of the deadline, whatever remaining challenges exist will need to be resolved in a hurry.
"You should probably call your insurance plan, the one you've believe you've enrolled in. Just verify that you've in fact enrolled," Laszewski says.
0 comments:
Post a Comment